Picture the traditional patient experience: a nervous individual calling a hospital landline, waiting on hold, scribbling information with pen and paper, juggling multiple forms, and perhaps arriving for an appointment only to face long queue times, crowded waiting areas, misplaced paperwork, or administrative delays. This analog world — familiar to millions — often created friction, stress, and a sense of disempowerment for patients.
Today, patients expect the ease and convenience they experience in other aspects of daily life — from booking a ride-share to ordering groceries — yet too often, the healthcare industry lags behind. As care providers and system leaders, this should give us pause: Are we still asking our patients to navigate a cumbersome, paper-based ecosystem, when we know better?
What if patients could book an appointment from their smartphone, receive confirmations instantly, upload basic information ahead of arrival, and use a secure portal to communicate and track care? The shift from landlines and paper forms to digital scheduling and patient portals is not just a convenience — it’s a patient-centric evolution. I invite you: how do you feel about the fact that many parts of the healthcare experience remain stuck in analog, even as consumer-grade technology has become ubiquitous?
The answer lies in embracing a broader, more holistic vision: one where digital tools support — and amplify — human empathy and touch at every step of the patient’s journey.
The transition to digital is not just a matter of convenience: it’s an evidence-based path to better patient engagement, satisfaction, and outcomes.
These figures underline a simple truth: when we lower administrative friction, patients feel more in control — and engage more. That sense of empowerment fosters trust, reduces anxiety, and paves the way for better long-term health outcomes.
Yet, implementing digital services is not enough by itself. As argued in recent research, the value of digital tools depends heavily on the context — especially patients’ digital literacy and access to technology. SpringerLink+1 This insight reinforces why the shift must be deliberate, inclusive, and rooted in an organizational commitment to patient-centered care.
To realize the full potential of digital engagement — without losing the human touch — we need to think beyond a single app or feature. That’s where the concept of a patient journey map becomes transformative.
A patient journey map is a holistic visualization of the patient’s experience from the very first moment they consider care, through diagnosis, treatment, discharge, and follow-up. It captures each touchpoint — clinical and non-clinical — including emotions, barriers, needs, decisions and interactions. IQVIA+2Viseven+2
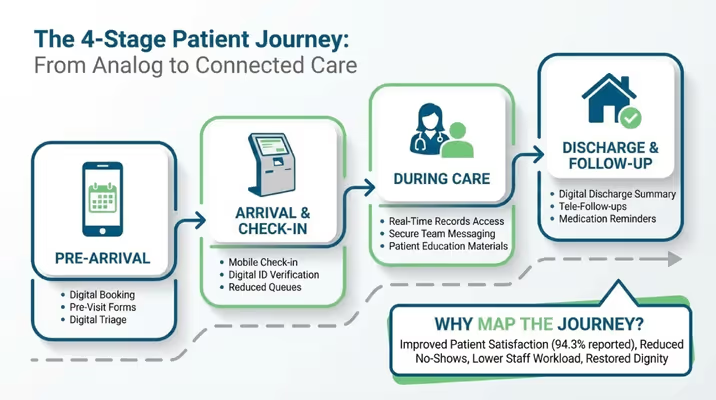
Rather than being a marketing gimmick, the journey map is a strategic tool. It helps us identify “moments that matter” — moments where interventions (digital or human) can make an outsized difference. For example:
Mapping the journey forces organizations to think broadly — not just about convenience, but about continuity, consistency, personalization, and empathy. It shifts care from episodic, transactional bursts to a continuous, patient-centered relationship.
As one practical guidance document puts it, a patient journey map integrates behavioral science, research insights, patient feedback, and organizational goals — building a bridge between what patients need and what the health system delivers. openhealthgroup.com+1
In essence: connected care is not just about digitizing one process — it’s about designing an ecosystem where every touchpoint is optimized for the patient’s needs and humanity remains central.
As someone who has implemented these approaches across multiple international health systems, my recommendation is simple:
Do not start with technology. Start with the journey.
Then introduce digital tools where they elevate human care — not where they merely automate tasks.
Ask your leadership teams:
Healthcare is not suffering from lack of technology. It is suffering from lack of connection. And connection requires design — intentional, compassionate, digitally enabled design.
When we do this well, we don’t just modernize systems.We restore dignity to the patient experience.