As healthcare professionals, we operate at the intersection of profound human need and exponential technological capability. Yet, why does so much innovation, designed to help us, often end up adding administrative burden, eroding caregiver time, and failing to engage the patient?
This problem, which the Connected Care methodology identifies as the "Curse of Intelligence," stems from prioritizing complex, high-cost solutions over the foundational wisdom of understanding the patient’s core struggle. When technology dictates that a physician must stare at a screen during a consultation, it actively detracts from the human connection essential for healing and trust.
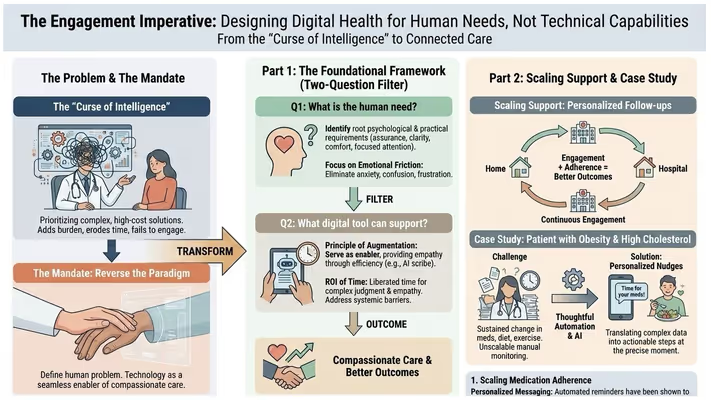
For healthcare leaders, policymakers, and clinicians committed to better outcomes, the mandate is clear: we must reverse the paradigm. True transformation begins with defining the human problem, allowing technology to act solely as the seamless enabler of compassionate care.
Before authorizing any new digital investment, leaders must filter the proposed solution through a rigorous, human-centered lens. The Connected Care framework offers two essential questions to anchor all innovation in purpose:
This question forces us to identify the root psychological and practical requirements of the user. For patients, the vital needs are assurance, clarity, comfort, and the focused attention of their caregiver.
Once the human need is defined, the role of technology is not to replace the professional, but to serve as the biggest enabler—providing empathy through efficiency.
Key Imperative: Technology must address systemic barriers to access. The Oregon Health & Science University (OHSU) observed lower rates of virtual (video) visit utilization among specific demographics (Black patients, non-English speakers, older adults) [https://www.chcs.org/resource-center-item/the-role-of-human-centered-design-in-healthcare-innovation-a-digital-health-equity-case-study/]. This shows that the technology itself was sound, but the delivery mechanism—the human-centered design—failed to account for essential equity needs.
The healing journey extends well beyond the hospital walls, operating in a continuous loop “from home, back to home”. Yet, traditional models create a massive disconnect post-discharge, driving poor adherence. This non-compliance is estimated to cost the U.S. healthcare system between $100 billion and $300 billion annually.
The Connected Care engagement formula is simple: Engagement + Adherence = Better Patient Outcomes. Technology is leveraged to scale continuous, empathetic coaching.
Managing chronic conditions like obesity and high cholesterol (dyslipidemia) requires sustained change across medication adherence, diet, and exercise. The core human need is continuous reinforcement and accountability. It is an unscalable human task for a clinician to manually monitor the daily weight fluctuations and medication compliance for hundreds of patients.
The solution utilizes thoughtful automation and AI to deliver personalized nudges at the precise moment they are needed, translating complex data into actionable steps:
1. Scaling Medication Adherence (Clarity and Reinforcement):
2. Driving Lifestyle Change (Objective Accountability):
The Outcome: This continuous feedback loop reinforces positive behavior change in real-time, effectively scaling the vital function of an expensive human health coach. The automation of mundane tasks frees the clinician to focus entirely on the complex human judgment that only they can provide: adjusting protocols, providing emotional support, and handling high-risk deviations.
The challenge is not one of technological capability; the tools for ubiquitous monitoring and seamless data flow exist. The true challenge is the philosophical commitment to ensure that technology remains the servant, not the master, of the care interaction. Lead with the human need, and the technology will follow.